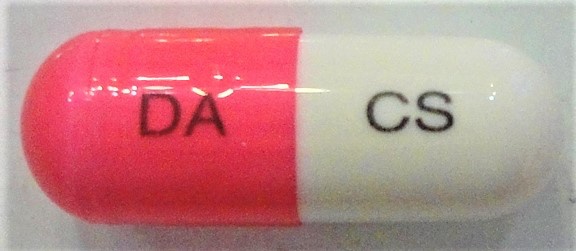
CLOSERIN Capsule
ក្រុមហ៊ុនផលិតឱសថ:
DONG-A ST, Korea
- សារធាតុសកម្ម
- ប្រសិទ្ធិភាពព្យាបាល និង កម្រិតប្រើប្រាស់
- ហាមប្រើ
- ផលរំខាន
- អន្តរប្រតិកម្ម
- ស្ត្រីមានផ្ទៃពោះ និង ស្ត្រីបំបៅដោះកូន
- ការប្រុងប្រយ័ត្នជាពិសេស បរិយាយប័ណ្ណឱសថ
-
សារធាតុសកម្ម
Cycloserine 250mg
-
ប្រសិទ្ធិភាពព្យាបាល និង កម្រិតប្រើប្រាស់
Susceptible microorganisms: Mycobacterium tuberculosis
Indication: in the treatment of active pulmonary and extra-pulmonary tuberculosis.
Dosage& Administration
Adults: The initial dosage is 250mg twice daily.
The dosage may vary according to the patient’s age and symptom.
In principle, Cycloserine is used in conjunction with other antituberculous agents.
-
ហាមប្រើ
1. Patients with hypersensitivity to Cycloserine
2. Patients with depression, epilepsy, severe anxiety of psychosis
3. Patients with severe renal insufficiency
4. Patients with excessive concurrent use of alcohol.
-
ផលរំខាន
1. Nervous system: headache, vertigo, drowsiness, tremor, depression, abalienatio, hallucination, coma, psychosis (possibly with suicidal tendencies), hyperreflexia, arthralgia, confusion, peripheral neuritis, paresis, dysarthria, hyposomnia, characteristic change, hyperirritability, aggression, paresthesia, major and minor (localized) clonic seizures, confusion and disorientation with loss of memory may occur. If the patient develops these symptoms, the administration should be discontinued.
2. Hypersensitivity: skin rash may occur. The administration should be discontinued of the dosage reduced if the patients develop allergic dermatitis.
3. Digestive system: occasionally, nausea, anorexia, abdominal pain, constipation, diarrhea may occur.
4. Cardiovascular: sudden development of congestive heart failure in patients receiving 1-1.5g of Cycloserine daily has been reported.
5. Hematologic: Vitamin B12 deficiency, folic acid deficiency, megaloblastic, anemia, and sideroblastic anemia may occur rarely in patients receiving Cycloserine in conjunction with other antituberculous agents. If anemia occurs, the patients should be sufficiency monitored and appropriate therapy should be initiated.
6. Other: elevated serum aminotransferase (transaminase) concentrations, especially in patients with preexisting liver disease, have been reported.
-
អន្តរប្រតិកម្ម
1. Concurrent administration of Ethionamide may potentiate neurotoxic side-effects, therefore the administration should be carried on the caution.
2. Alcohol increases the possibility and risk of epileptic episodes, therefore it should be avoided during treatment.
3. Concurrent administration of isoniazid may result in increased incidence of CNS effects, such as dizziness or drowsiness. Dosage adjustments may be necessary and patients should be monitored closely for signs of CNS toxicity.
-
ស្ត្រីមានផ្ទៃពោះ និង ស្ត្រីបំបៅដោះកូន
1. Safety in use in pregnancy has not been established. Therefore, it should only be used in pregnant women or women with potential to become pregnant only if the expected benefits to the mother exceed the potential risk to the fetus.
2. It has been reported that the drug was excreted in the milk. Therefore, mothers who are under treatment should not breast-feed.
-
ការប្រុងប្រយ័ត្នជាពិសេស
The drug should be cautiously administered in the following patients
1. Patients with renal impairment
2. Patients with a family history of psychosis or epilepsy
3. Alcoholics
4. Patients with allergic skin infections, confusion, hyperrflexia, headache, chills, dizziness, incomplete paralysis, dysphemia, etc… symptoms of central nerve toxicity.
5. This pharmaceutical product contains yellow no.5 (sunset yellow FCF), therefore it should be administered with caution to patients who are sensitive to it, or who have allergic medical history to yellow no.5.
General precautions
1. Prior to the administration of Cycloserine, susceptibility to the drug should be tested to prevent manifestation of resistant bacteria and the duration therapy should be the minimum of needed for the treatment.
2. Cycloserine is used after failure of adequate treatment with the primary medications (streptomycin, isoniazid, refampicin and ethambutol).
3. The toxicity of Cycloserine is closely relate to excessive blood levels (above 30µg/mL), as determined by high dosage or inadequate renal cleance. The ratio of toxic dose to effective dose in tuberculosis is low.
4. Patients with hepatic, renal impairment should be monitored by hematologic, renal excretion, blood level, and liver function studies.
*ព័ត៌មានឱសថត្រូវបានរៀបរៀងដោយ អ៊ីម៉ាតុគឹ មេឌីក (ខេមបូឌា) ដោយផ្អែកលើប្រភពព័ត៌មានខាងក្រោម។ សម្រាប់ព័ត៌មានលម្អិត សូមស្វែងរកនៅក្នុងក្រដាសព័ត៌មាននៃឱសថនីមួយៗ ឬ សាកសួរទៅកាន់ក្រុមហ៊ុនឱសថឬតំណាងចែកចាយនៃឱសថនីមួយៗ។
ប្រភពព័ត៌មាន៖
- ក្រដាសព័ត៌មាននៃឱសថសម្រាប់អ្នកជំនាញវេជ្ជសាស្ត្រដែលប្រើប្រាស់នៅប្រទេសជប៉ុន (Pharmaceutical and Medical Devices Agency, Pmda): https://www.pmda.go.jp
- ព័ត៌មានសង្ខេបនៃឱសថសម្រាប់អ្នកជំងឺដែលប្រើប្រាស់នៅប្រទេសជប៉ុន: http://www.rad-ar.or.jp
